When we think about the immune system, most of us picture white blood cells fighting off a cold or healing a cut. But here’s something crucial to keep in mind: your brain has its own immune system that works entirely different than the rest of your body.
As the CAD Foundation funds research into the microbial / infectious hypothesis of Alzheimer’s, this idea of the brain having its own immune system is very important. Especially in instances where something foreign ( environmental toxin or even a bacterial, viral, or fungal cell ) gets past the blood brain barrier where it’s not supposed to be.
You’d be lost if your brain didn’t have its own immune system. Literally.
Instead of white blood cells, your brain uses immune cells called microglia to monitor, protect, and support its neurons. Microglia are essential for keeping neurons healthy — and alive. When neurons become sick or die, it affects how we think, feel, and function. That’s why keeping them safe is so important.
Let’s break the brain’s immune system down cell by cell. And then look at what happens when things go awry.
What Are Glial Cells?
Microglia are just one type of glial cell — they are a group of non-neuron cells that play critical support roles in the brain. While neurons do the thinking, glial cells keep everything running smoothly. They provide structure, deliver nutrients, clean up waste, and help defend the brain. Interestingly, glial cells outnumber neurons in many parts of the brain.
The word “glia” means “glue” in Greek—but they do way more than just hold things together.
There are several types of glia, but for brain cleaning and immune function, the most important are:
- Microglia: The immune cells of the brain. They detect threats like infections or debris and send out cytokine alerts to coordinate a response.
- Astrocytes: Star-shaped cells that help with repair, maintain the blood-brain barrier, and regulate nutrients and neurotransmitters. They’re also key players in waste clearance and play an important role in the brain’s advanced immune system by releasing and responding to cytokines, helping to coordinate inflammation and protect neurons.
Microglia are essentially the Brain’s Bodyguards
Astrocytes are the Brain’s Support Team and Maintenance Crew
Meet the Microglia: Bodyguards Extraordinaire
These tiny (thus the term micro), spider-shaped cells are basically the brain’s built-in security guards. They’re constantly patrolling, looking for anything that shouldn’t be there ( dead cells, waste products, misfolded proteins, excess neurotransmitters and pathogens ). If they find any of these “problems” in the brain, they sound the alarm and start cleaning things up.
But microglia aren’t just there for emergencies. They also help keep your brain working smoothly by pruning weak or unused connections between brain cells. Kind of like a gardener trimming branches to help the tree grow better.
Astrocytes: The Helpers That Do Everything
Astrocytes are larger than micogroglia and more star-shaped, with long, branching arms that spread out to support and connect many neurons at once. They act like the brain’s caretakers, overseeing and maintaining the environment where neurons live and work. Here are some of their chores:
- They bring nutrients to your brain cells.
- They help control what gets in and out of your brain’s blood supply.
- They even clean up chemical messes after brain cells “talk” to each other. We often refer to this as the “metabolic debris” that accumulates all day long as you walk, talk, think, eat and read your best friend’s Facebook post about her new kitten.
Astrocytes are like backstage crew at a concert—if they weren’t there, the show wouldn’t run.
Learning & Healing: BDNF and Cytokines
So we were just talking about cells a moment ago. But another important player in your brain’s immune system are molecules. Keep in mind: cells are anywhere from 1,000 to 100,000 times larger than molecules. But smaller size doesn’t mean less power. Let’s learn more about two very important molecules used by the brain’s immune system.

BDNF (brain-derived neurotrophic factor) is a mouthful, but think of it as Miracle-Gro for your brain. It helps your brain grow, heal, and learn. You make more BDNF when you exercise, sleep well, or challenge yourself to learn something new. Interestingly, and to be discussed in greater detail – chewing your food well boosts BDNF levels!
BDNF doesn’t just help your brain grow — it also helps keep inflammation in check. When BDNF levels are healthy, it protects neurons from stress and reduces the risk of overactive immune responses in the brain. Low BDNF has been linked to higher inflammation, brain fog, and mood issues. In a way, BDNF helps keep the brain’s immune system balanced — encouraging healing, not harm.
Cytokines – which are also tiny molecules in your brain – can be thought of as “text messages” your immune system uses to send alerts. Some are anti-inflammatory—they help calm things down and keep your brain balanced. They work in harmoney with BDNF.
Other types of cytokines are actually pro-inflammatory—they jump into action when there’s a threat, like you’d find with an infection. But when your body sends too many of the wrong (text) messages (especially during stress, poor sleep, or chronic infections), it creates ongoing inflammation in the brain. That kind of constant “brain fire” can damage brain cells and make it harder to think clearly or remember quickly or even remember at all.
So, who sends out these cytokine alerts?
Think of your brain like a high-tech city. When there’s trouble—like a virus sneaking in, a head injury, or a long-term bacterial infection (like see with gum disease)—your brain’s security guards (remember the microglia from earlier?) sound the alarm. Microglia are like firefighters and paramedics rolled into one. They scan the scene, then call for cytokines to come and check it out.
Some cytokines – are just informational…
“Hey, there’s a mess to clean up.”
Others hit the panic button and scream…
“This is serious!”
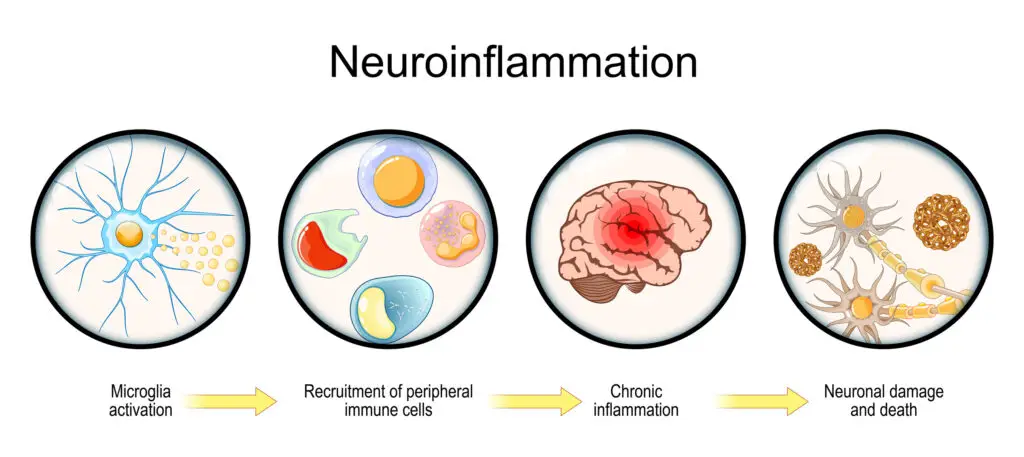
…in effort to bring in heavy reinforcements. If it’s a quick fix—like clearing out a dying cell—the cytokine response wraps up fast. But if the problem is ongoing and unresolved, like with chronic bacterial infection, the alerts don’t stop. The emergency system keeps firing, and eventually, it goes haywire. Instead of helping, it starts harming healthy brain cells—causing swelling (inflammation), confusion, and over time, even memory loss.
And then there’s the Night Crew: The Glymphatic Team who clean while you sleep
Ever wonder why sleep is so important? Well, while you’re deep asleep, your brain uses it’s own type of cleaning system to collect and flush out waste, including that metabolic debris mentioned earlier as well as any other “junk” left behind by immune battles that took place during your day.
It’s called the GLYMPHATIC SYSTEM. Think lymphatic (which in the body is how we remove impurities) just this system starts in your brain and is powered by glial cells.
Eventually, the glymphatic system dumps the misfolded proteins, toxins, debris, and dead cells off to the body’s lymphatic system so it can finish removing all that garbage
We will go into greater depth in a later post, but for now, just realize that your brain literally cleans itself at night. That’s why pulling an all-nighter can leave you feeling foggy and slow.
When the Brain’s Immune System Goes Wrong
But just like any system, things can break down. If microglia or astrocytes go into overdrive—or if your body sends too many inflammatory cytokines to the brain—it can cause problems. Scientists think this may play a role in conditions like Alzheimer’s Disease.
As a quick review:
- Your brain has its own immune system, separate from the rest of your body.
- Glial cells = the brain’s behind-the-scenes support team (includes microglia & astrocytes).
- Microglia = bodyguards & clean-up crew (they fight infections and eat up debris).
- Astrocytes = support squad & chemical managers (they guide nutrients and help with brain detox).
- BDNF = brain fertilizer; helps neurons grow and form new connections.
- Cytokines = immune text messages; helpful alerts in small amounts, harmful when constant.
- Glymphatics = the brain’s night shift janitors; they flush out toxins, mostly during deep sleep.
So, if you want your brain to stay sharp: sleep, move, learn, and chill out. Your brain’s immune squad will thank you.
We are hoping this overview of the brain’s immune system is helpful when understanding how long-term infections—like those caused by gum disease—might quietly spark this immune overreaction that leads to Alzheimer’s.
articles to check out:
- Mechanistic insights into the role of amyloid-β in innate immunity 2024 Journal of Nature Tatum Prosswimmer, Anthony Heng & Valerie Daggett https://www.nature.com/articles/s41598-024-55423-9
ABSTRACT: Colocalization of microbial pathogens and the β-amyloid peptide (Aβ) in the brain of Alzheimer’s disease (AD) patients suggests that microbial infection may play a role in sporadic AD. Aβ exhibits antimicrobial activity against numerous pathogens, supporting a potential role for Aβ in the innate immune response.
2. In 2024, the amyloid-cascade-hypothesis still remains a working hypothesis, no less but certainly no more 2024 Frontier Christian Behl* https://www.frontiersin.org/journals/aging-neuroscience/articles/10.3389/fnagi.2024.1459224/full
CONCLUSION: Interestingly, the amyloid-cascade-hypothesis is a prime example for an idea presented by the philosopher Thomas S. Kuhn on trajectories of scientific paradigms (Kuhn, 1970). Kuhn’s discerns three key phases in science and in the evolution of scientific progress: (1) the preparadigmatic phase of science (competing views and approaches exist), (2) the paradigmatic phase of science (one particular paradigm dominates field), and (3) the revolutionary phase (certain inconsistencies and anomalies trouble the current theory, which is attacked and under pressure; novel views appear). This ultimately culminates in a paradigm shift and a scientific revolution. Regarding the amyloid-cascade-hypothesis, I would say, we are not quite there yet; we have not reached the final steps of stage 3, the necessary paradigm shift. Very likely, it will take more time to get there, and the amyloid-cascade will continue to be the basis of many basic, preclinical, and clinical research which is already ongoing or planned. Yet, in my personal view and as written in the headline of this discussion, in 2024, the amyloid-cascade-hypothesis still remains a working hypothesis—no less but certainly no more.
DISCLAIMER
No content on this site, regardless of date, should ever be used as an absolute substitute for direct medical advice from your doctor or other qualified clinician. This article should be viewed as advice that is based on current research regarding the potential to slow and possibly prevent Alzheimer’s Disease.
Copyright © 2022 Curing Alzheimer’s Disease [EIN #88-3154550] All Rights Reserved. This information is not designed to replace a physician’s independent judgment about the appropriateness or risks of a procedure for a given patient. Always consult your doctor about your medical conditions. Curing Alzheimer’s Disease.com does not provide medical advice, diagnosis or treatment. Use of the site is conditional upon your acceptance of our terms of use.