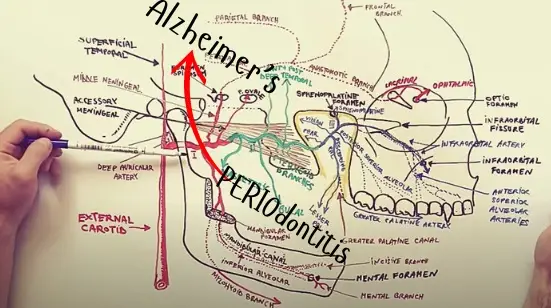
If we described Periodontal Disease, you’d think we were describing Alzheimer’s.
Just like Alzheimer’s, Periodontal Disease (PD) is painless and often goes undetected until damage has already occurred. And just like with Alzheimer’s: PD is a disease of inflammation.
Periodontal Disease is an age-related disease
PD is also considered an age-related disease – increasing in incidence the older you are. Periodontal Disease is also increasing in incidence worldwide. Babies don’t get it. Kids don’t get it. Teens don’t get it. It starts to be a “thing” in our late twenties and increases in frequency the older we get.
Periodontal Disease develops silently - over a VERY long period of time
Literally, no one with Periodontal Disease knows they have it. And most dental healthcare teams aren’t really comfortable sharing this “dirty secret” with their patients – even though we now know it’s not dirty at all. It’s contagious. By natural life events such as sharing eating utensils, drinking from the same cup, or kissing.
FINALLY: Finding a Bacterial Balance
Are we helpless to this? Absolutely not! But we need to be empowered with knowledge first and foremost. We need to understand the underlying mechanism(s) of action on this serious condition that could be causing Alzheimer’s.
The bacteria in your mouth, like what we are finding to be true of the bacteria in your gut, needs to be balanced to support optimal health. Unfortunately, just as we find with our colon – [which, by the way is at end of the same canal (the alimentary canal that begins in the mouth and ends at the rectum)] – when your oral bacteria (or gut bacteria) becomes imbalanced by an overpopulation of “bad” bacteria – bigger and bigger problems arise.
We all carry bacteria in our mouths — and that’s not a bad thing. In fact, many types of bacteria (along with viruses and fungi) are essential for digesting food and keeping our oral microbiome balanced. Ideally, your “good” microbes outnumber the harmful ones, which is how your mouth and body stay healthier.
But when harmful bacteria are left unchecked, they multiply and begin to break down gum tissue as they search for nutrients and, eventually, a blood source.
As this process continues, the infection can spread below the gum line and into the jawbone itself. Over time, the bacteria don’t just damage soft tissue — they also contribute to bone loss, which is why periodontal disease often shows up as jawbone loss on dental x-rays.

Gum disease — also known as periodontal disease — often starts subtly. Early warning signs include bleeding when you brush or floss, gums that look red or swollen, or tenderness around the teeth.
The bacteria that drive this disease are “anaerobic,” meaning they thrive where oxygen is limited — often in the deep pockets around your back molars. If left untreated, the infection spreads, creating more inflammation that pushes below the gum line. Over time, these bacteria damage the periodontal ligaments — the structures that anchor your teeth — leading to “detachment.” This is when a tooth becomes loose or mobile, and if the process continues, the tooth may eventually be lost.
What’s happening beneath the surface can be even more concerning. The same bacteria and inflammation that destroy gums and bone can enter the bloodstream through tiny blood vessels in the gum tissue. From there, they don’t just stay in the mouth — they can travel to other parts of the body, where ongoing research suggests they may play a role in systemic conditions, including heart disease and possibly even brain health.
It is very important to understand that bleeding gums is not normal/natural from ordinary things like: teeth brushing, flossing or eating.
What's the CDC Have to Say?
According to the CDC, nearly half of adults over age 30 show some form of periodontal disease — and by age 65, that number climbs to about 70%. What often surprises people is that the bacteria involved can be passed from person to person through everyday contact such as sharing utensils or even a kiss.
Now here’s the critical connection: while not everyone with gum disease will go on to develop Alzheimer’s, studies consistently show that more than 70% of individuals with Alzheimer’s also have periodontal disease. This overlap raises an urgent question: what role might chronic oral infection play in brain health?
That is exactly the question driving the research at The Alzheimer’s Legacy Lab. Our foundation is the sole funder of this work — work that is now advancing from animal models toward published results. With your support, we are helping uncover whether treating periodontal disease could also slow or alter the course of Alzheimer’s disease.
The relationship between tooth loss and cognitive decline is “dose-dependent”
In a 2021 study, researchers discovered a 1.4% increase in the risk of mild cognitive impairment (MCI) with each lost tooth and a 1.1% increase in the risk of generalized dementia. Participants who were missing 20 (or more) teeth had a 31% higher risk of cognitive impairment and/or dementia.
And there's some real science to this: Tooth extractions allow oral bacterial to get into the blood stream and into the brain

When a tooth is extracted, it leaves behind a deep opening that can take months to fully heal — anywhere from 3 months to over a year. Healing slows as we age, and conditions like diabetes stretch that timeline even further. The longer the site stays open, the more opportunity harmful oral bacteria have to enter the bloodstream through tiny vessels in the socket. Once in circulation, those bacteria don’t stop — they can travel to distant parts of the body, including the brain.
This helps explain why tooth loss is linked with higher dementia risk. Each lost tooth raises that risk, and older adults are especially vulnerable. It’s no coincidence that so many living with Alzheimer’s also rely on dentures. The overlap is striking, and it underscores an important prevention tip: whenever possible, work with your dentist to save your natural teeth.
Periodontal Disease = Tooth Loss
Many adults lose teeth to injury or break down. But Periodontal Disease (PD) remains the number one cause of tooth loss in the adult population. In looking at Alzheimer’s Risk Factors – you’ll see that Periodontal Disease is in the top 5 comorbid conditions for AD. Why is that?
Visit this article on the connection between tooth loss and AD
One Final Note
At some point, dentistry will need to address this connection between tooth loss and dementia straight on and begin looking for ways to substantially reduce the opportunity for oral bacteria to get into the blood stream following an extraction.
One way is to shorten wound healing time.
And not surprising, researchers are already discovering some exciting new options that one day soon may be available at a dental clinic near you.
For one, Platelet-rich Plasma (PRP) is a very viable healing option, and now we are finding promising results with a new procedure using Platelet-rich fibrin (PRF) in the extraction site to speed up wound healing. This 2018 study found that “an appreciable wound healing and bone regeneration was seen in the experimental group when compared to the control sites where no PR was used substantiating the use of PRF as an inexpensive autologous material for socket preservation and future rehabilitation. The present study, also, showed that minimal operator expertise was required to conduct the procedure of PRF preparation and grafting when compared to bone harvesting from distant sites.” The study noted that using PRF shortens the time between extractions and implant placement and eliminates the need for secondary procedures prior to final restoration.
And something as simple as honey could be an option: In this 2019 study using Honey as a wound-healing support after extractions, the significant healing observed caused the researchers to conclude: “Honey resulted in a decrease in wound sizes and faster healing after extraction of teeth in children. Therefore, use of honey can be recommended after minor surgeries in the oral cavity.”
And for the slower healing diabetics, researchers in this 2020 study found that 0.8% hyaluronic acid placed in post-extraction socket in patients with poorly controlled diabetes may improve wound healing, especially in the first days after application. As we learn more on this novel option to encourage wound healing (and therefore reduce risk oral bacteria translocating to the brain) we will likely share it in a future blogpost.
And as the world realizes that no mature tooth extraction is “simple” and that all extractions come with dementia risks, perhaps we will see even more inroads in extraction wound healing to come!
Our Minnesota Foundation – The Curing Alzheimer’s Disease Foundation – is all about preventing Alzheimer’s while the world works to find a cure.
No content on this site, regardless of date, should ever be used as an absolute substitute for direct medical advice from your doctor or other qualified clinician. This article should be viewed as advice that is based on current research regarding the potential to slow and possibly prevent Alzheimer’s Disease.
Copyright © 2022 Curing Alzheimer’s Disease [EIN #88-3154550] All Rights Reserved. This information is not designed to replace a physician’s independent judgment about the appropriateness or risks of a procedure for a given patient. Always consult your doctor about your medical conditions. Curing Alzheimer’s Disease.com does not provide medical advice, diagnosis or treatment. Use of the site is conditional upon your acceptance of our terms of use.