The Alzheimer’s Legacy Lab is Growing!
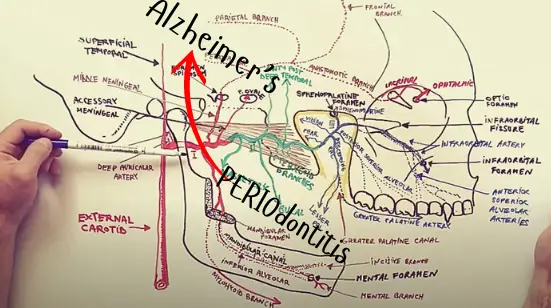
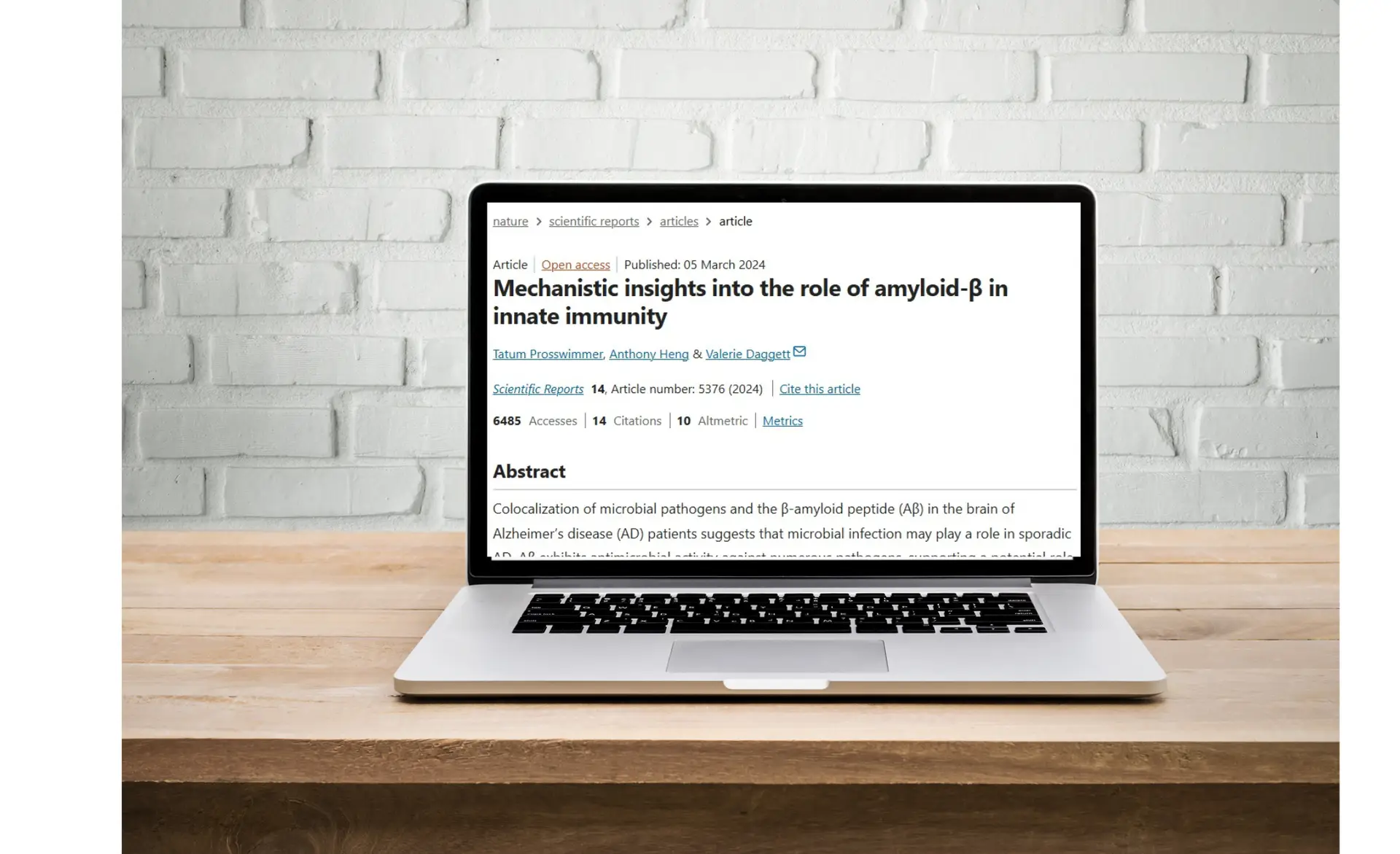
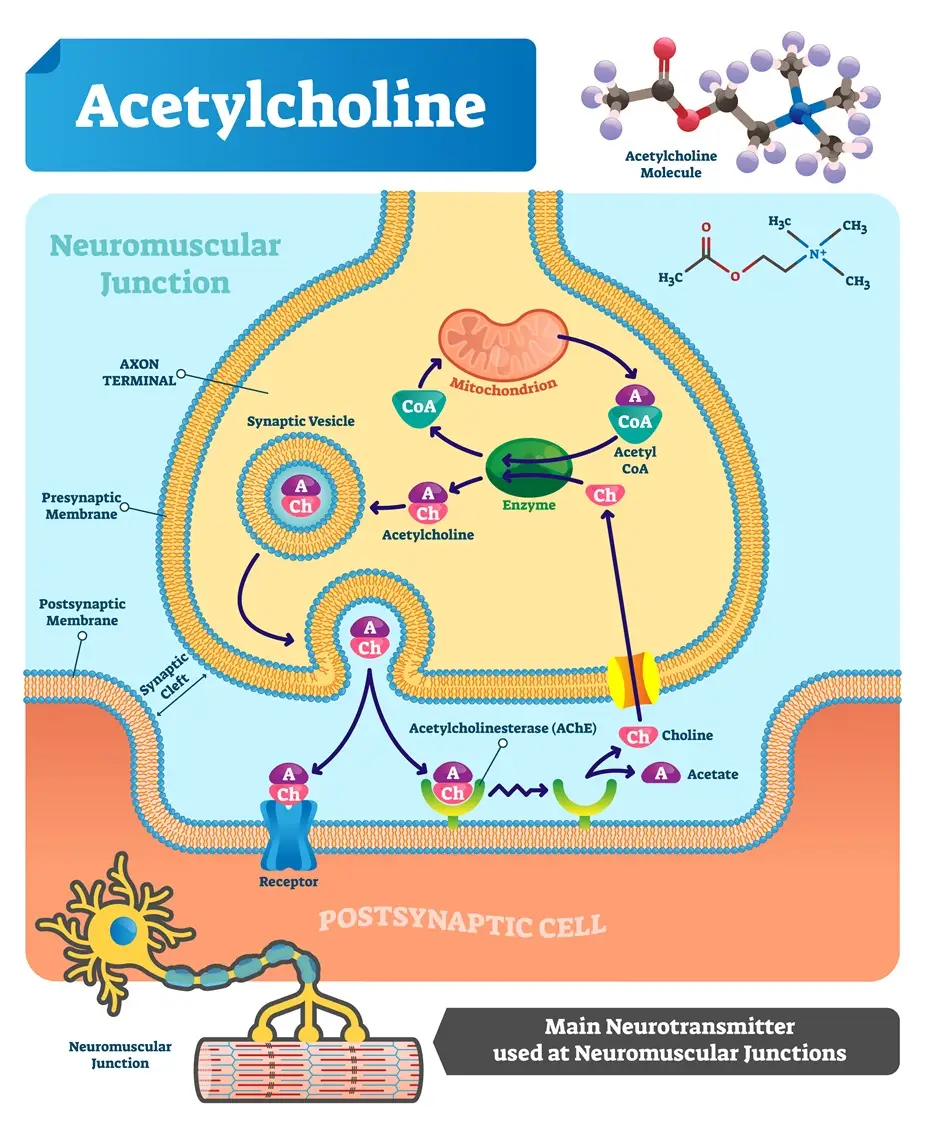
Five World Class Scientists –One Exceptional Lab The Alzheimer’s Legacy Lab continues to grow. Back in 2022, when we began this journey of funding an Alzheimer’s research lab at the University of Minnesota, our team was dedicated—but small. It consisted of Dr. Liam Chen, who heads the Neuropathology Department (and also teaches and serves on the Medical School’s administrative team), and me. At the time, Dr. Chen reluctantly admitted that the NIH would not be funding his work on the Microbial/Infectious Hypothesis of Alzheimer’s Disease (MAD). And without funding, he explained, a lab could not be opened and I may as well have my dad’s brain back.In that moment, the idea my dentist-dad and I had talked about many times before … came to life: What if I raised the money myself to fund this critical work?Hundreds of hours—and thousands of dollars—later, the CAD Foundation was born and over the next year we entered into a Sponsored Projects Agreement [SPA] with the University of Minnesota Medical School. This unprecedented agreement holds our feet to the fire. We are contractually obligated to fund the lab until the scientists fully explain the irrefutable overlap between Alzheimer’s disease and periodontal disease (and other infections within the human body) and how we can stop these infections from causing harm to the brain. We also differentiated ourselves further by agreeing to pay all administrative costs of the research work ourselves – PLUS we agreed that the researchers can pivot their research – provided the CAD Foundation’s scientific committee agrees the change is warranted. Already this has occurred — and as a result, we were able to shave 12 months off the lab’s timeline! As we near the end of 2025, we’re excited to share that The UMN Alzheimer’s Legacy Lab now has deep, committed, and highly capable support—1) within the lab 2) across the CAD Foundation and 3) with our funding partners: YOU. This blog post is our way of keeping you informed about the growth and accomplishments of the scientific team that are making this progress possible… Meet Liam Chen M.D. PhD Dr. Chen is a nationally respected neuroscientist and neuropathologist whose work focuses on understanding what causes neurodegenerative diseases, including Alzheimer’s and Parkinson’s.He is a faculty member at the University of Minnesota, where he leads research exploring the biological mechanisms that drive brain degeneration. Dr. Chen trained at top institutions around the world, earning his medical degree in China, completing a PhD in genetics in Canada, and finishing advanced pathology and neuropathology training at Harvard Medical School.His research has been published in leading scientific journals, including Nature and the Journal of Alzheimer’s Disease, and he is also an inventor, holding a patent related to proteins involved in Alzheimer’s and other neurodegenerative disorders.In addition to his research, Dr. Chen serves in leadership and mentoring roles within the scientific community, helping guide the next generation of researchers. His experience, global training, and proven track record make him uniquely qualified to lead innovative Alzheimer’s research. Meet Na Yin, PhD. Dr. Yin is an accomplished research scientist and the heart of the lab’s operations. With 15 years of experience in translational research spanning neuroscience and oncology, she brings a wealth of technical expertise and leadership to every project. Na is skilled in advanced techniques including proteomics, genomics, and a variety of molecular and biochemical assays, ensuring that all experiments are executed with precision and rigor.Beyond her technical skills, Na excels at fostering collaboration, mentoring team members, and communicating complex scientific findings clearly—whether in academic publications or presentations. Her dedication and organizational talent keep the lab running smoothly, making her an indispensable part of the CAD Foundation’s mission to accelerate Alzheimer’s research. Meet Javier Redding-Ochoa, MD. Dr. Redding-Ochoa is a physician–scientist trained in anatomic pathology with deep expertise in neuropathology and neurodegenerative disease. He earned his medical degree in Mexico City and completed a full residency in anatomic pathology at one of Mexico’s leading national medical institutes.Since 2019, he has examined more than 500 human brains, developing rare hands-on expertise in neurodegeneration, forensic neuropathology, and brain banking. He completed advanced postdoctoral research training at Johns Hopkins School of Medicine in the laboratory of Dr. Juan Troncoso, a nationally recognized leader in neurodegenerative disease research.At Johns Hopkins, he worked across both clinical and research settings, contributing to multiple collaborative studies from experimental design through publication, and gaining experience running a brain tissue repository—a critical asset for translational Alzheimer’s and neurodegeneration research.He is also an experienced educator, having delivered lectures to neurology residents, taught medical students in neuropathology workshops, and led specialized forensic pathology training for fellows and international pathologists.Driven by a commitment to patient-centered science and discovery, his career focus is on neuropathology, neurodegenerative disease, and translational research, with the goal of advancing understanding and treatment of disorders such as Alzheimer’s disease. Meet Han Tong MD PhD. Dr. Han Tong is a board-certified surgeon and neurodegeneration researcher with expertise in both general surgery and surgical critical care. Before joining the Alzheimer’s Legacy Lab, he contributed to cutting-edge Alzheimer’s research at Rice University’s Alzheimer’s Disease Research Center, where he studied how the developing brain processes pain and explored structural brain changes linked to neurological conditions.Dr. Tong’s work bridges clinical care and neuroscience research, with publications in leading journals such as Pain, Journal of Integrative Neuroscience, and Arthritis & Rheumatology. He brings a deep understanding of neurodegenerative processes and a commitment to advancing research that could inform treatments and preventative strategies.As a member of the American Academy of Neurology, Dr. Tong strengthens the lab’s mission by applying his expertise to uncover the underlying mechanisms of Alzheimer’s and related brain conditions, helping accelerate breakthroughs in neurological health. Meet Dr. Chuanyin Hu Dr. Hu, a highly skilled translational neuroscientist from Guangdong Medical College in Zhanjiang, China, joins the Alzheimer’s Legacy Lab in March 2026 to lead their comprehensive animal study—a central component of our research program. Her work includes animal models and in‑vivo studies relevant to neurodegeneration, inflammation, and nervous system function. She has co‑authored peer-reviewed research using rodent models to investigate neurological and behavioral outcomes related to oxidative stress, neuroinflammation, and apoptosis—all key
The Alzheimer’s Legacy Lab is Growing! Read Post »